Last Updated on June 3, 2023
What is Rheumatoid Arthritis?
Rheumatoid arthritis is a chronic (long lasting) inflammatory disease that causes pain, stiffness, warmth, redness and swelling in joints. Over time, the affected joints may become misaligned, misshapen and damaged. Tissue lining the joint can become thick, and could wear away encompassing bone, cartilage and ligaments as it spreads. Rheumatoid arthritis generally occurs in a symmetrical pattern, meaning that if one knee or hand has it, the other generally does, also.
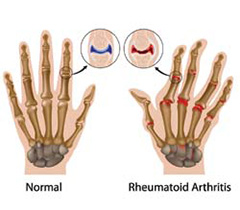
The reason for rheumatoid arthritis is unknown, though it seems to be an autoimmune disease. White blood cells that normally attack bacteria or viruses attack healthy tissue in this case, the synovium, or joint tissue when the body’s immune system will not work as it should. Over time, immune cells that are certain and these enzymes damage the cartilage, bone, tendons and ligaments near the joint.
Some research suggests a virus triggers this immune response that is faulty. Yet, there’s not yet convincing evidence that a virus is the cause of rheumatoid arthritis. At precisely the same time, it seems that some folks are far more prone to get the disorder due to their genetics. Environmental factors are often significant.
The most disabling form of arthritis, rheumatoid arthritis, usually affects more than one joint at a time. Rheumatoid arthritis can result in loose, deformed joints, loss of mobility and diminished strength. In addition, it can not cause painful lumps the size of a pea or acorn , called rheumatoid nodules. These grow under your skin, especially across the elbow or beneath the toes.
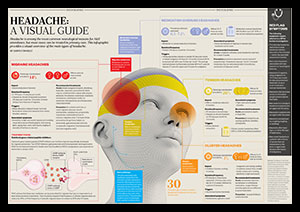
Generally, the pain of rheumatoid arthritis is called a dull ache, not dissimilar to that of toothache or a headache. Pain is typically worse in the morning. It’s not uncommon to have 30 minutes to one hour or even more of morning stiffness. On days when the illness is more active, you can experience loss of appetite, fatigue, low-grade fever, sweats and difficulty sleeping.
Because rheumatoid arthritis is a systemic disorder (meaning it can affect the whole body), in addition, you may have inflammation in other places, such as the heart, lungs or eyes. Symptoms vary between individuals and even in one single person over time. They may well not experience any joint damage, although people with moderate types of the disease are disturbed by pain and stiffness. For others, damage happens early, requiring aggressive medical and surgical treatment. People who have rheumatoid arthritis may notice advancement and worsening for no obvious reason. Although this disease most often afflicts people between the ages of 50 and 20, it could impact the elderly and children. Of the 2 million people with rheumatoid arthritis in the United States, at least 75 percent are girls.
Symptoms
- Weakness and loss of freedom
- Depression
- Pain, swelling, limited motion, heat and tightness in a symmetrical pattern, generally around affected joints, which most commonly range from the hands and wrists, feet and ankles, elbows, shoulders, neck, knees and hips.
- Fatigue, soreness, stiffness and aching, particularly in the morning and afternoon (described as morning stiffness and afternoon fatigue)
- Low-grade fever and sweats
- Trouble sleep
Identification
Your doctor will ask about your symptoms and medical history, and will examine you. Additionally you might be sent for a blood test. Yet, having RF does not always mean you have rheumatoid arthritis. Many individuals who do not have rheumatoid arthritis can have RF appear in their blood.
A more lately accepted antibody, called the anti-cyclic citrullinated protein (anti-CCP), is a more specific indication of rheumatoid arthritis. While it is less general, the diagnosis of rheumatoid arthritis cannot be based solely on a blood test that is positive for anti-CCP. Other blood tests may be performed to check if liver and the kidneys are working generally and also to look for some other causes of joint pain, anemia.
You might learn in regards to a checklist of symptoms (called criteria) for diagnosing rheumatoid arthritis. It is essential to understand that some patients with rheumatoid arthritis tend not to have lots of the symptoms on the list, especially if their disease is mild although some doctors use this checklist as a guide. Plus some people with other forms of arthritis may fulfill standards for rheumatoid arthritis.
The identification of rheumatoid arthritis relies mostly on the expertise as well as judgment of the physician, and is founded on the “big picture” of symptoms, examination and test results.
Expected Duration
Most individuals with rheumatoid arthritis have long-term (long lasting) symptoms. They experience periods when symptoms get worse, called flare ups, and periods when symptoms improve. Rarely, symptoms and signs of the disease disappear, called a remission.
Prevention
There’s absolutely no method to avoid rheumatoid arthritis. So this is one more reason not to smoke.
Treatment
The treatment of rheumatoid arthritis has improved drastically in the past 50 years. A comprehensive strategy that joins drugs, rest balanced with exercise, lifestyle adjustments, and sometimes surgery, can help many individuals to lead normal lives. The most important targets in treating rheumatoid arthritis are keeping your capability to function and move, reducing pain, and preventing future joint damage. Quality of life and period of life may be normal, if these are achieved. The treatments may cause difficulties. You as well as your doctor must weigh the risks and benefits of any drug or alternative treatment that’s available for this particular disorder.
Medications
Particular medications relieve the symptoms of rheumatoid arthritis (for example pain and swelling), while other medicines slow the progress of the illness.
Unwanted side effects occur in a minority of patients. These include allergy symptoms, ulcers, reduced kidney function or upset stomach.
Newer NSAIDs, including celecoxib (Celebrex), may provide the same advantages for arthritis as old drugs but with less risk of ulcers. On the other hand, the chance of ulcers is not zero. One study revealed that for people at highest risk (those with recent bleeding ulcer), up to 10 percent of these treated with celecoxib developed a brand new ulcer. Furthermore, the risk was similar for these high-risk patients taking celecoxib and those taking an older agent (Diclofenac) along with the acid blocker Omeprazole.
Corticosteroids, such as Prednisone (Deltasone along with other brand names), reduce inflammation. Nevertheless, they have little lasting benefit and come with a very long record of troubling side effects, including easy bruising, thinning of the bones, cataracts, weight gain, puffy face, diabetes and high blood pressure, amongst others. Follow your physician’s recommendations should you use corticosteroids. Your physician may prescribe a corticosteroid to relieve occasional flareups, and after that slowly taper you off the medication. Discontinuing corticosteroid treatment suddenly may not be safe.
Disease-modifying antirheumatic drugs (called DMARDs, second-line drugs or remittive therapy) seem to slow or prevent the progression of rheumatoid arthritis by changing the function of your body’s defense mechanisms. Most specialists recommend that all individuals with rheumatoid arthritis take a DMARD shortly after being diagnosed to lessen the likelihood of joint damage. These medications take time to begin working. Because these medications take some time to start working, your doctor probably will advise you to take an NSAID, a corticosteroid or both throughout the early weeks or months of treatment with a DMARD.
These drugs include Methotrexate (Folex, Methotrexate LPF, Rheumatrex), hydroxyChloroquine (Plaquenil), leflunomide (Arava) or Sulfasalazine (Azulfidine). Treatment typically includes Methotrexate as the first pick but blends of the drugs (e.g., Methotrexate, hydroxyChloroquine and Sulfasalazine) are often prescribed. Each of these comes with a tiny risk of serious side effects. Your doctors will review them.
Newer medications, called “biologics” comprise:
- adalimumab (Humira)
- golimumab (Simponi)
- infliximab (Remicade)
- rituximab (Rituxan)
- tocilizumab (Actemra)
- tofacitinib (Xeljanz)
Except for tofacitinib (a new oral medicine), these medicines are offered by injection only. They are able to be impressive, but a lot of patients improve with older drugs which are not as expensive, so older treatments are recommended by most physicians first.
Another drug for rheumatoid arthritis is anakinra (Kineret), an injectable drug that is apparently only modestly successful but can be a practical alternative if other treatments have failed. Nevertheless, these treatments are employed much less often because most specialists discover that they are much less powerful or safe.
Because the newest medicines have been studied just in chosen, and frequently the most healthy, people, they might have negative effects that are not yet well-known. By way of example, new dangers were found for infliximab two or a year after it was approved to be used. Studies found that tuberculosis, although uncommon, was more common than expected among those receiving treatment. In a trial of infliximab treatment for congestive heart failure, in addition, a higher death rate was found compared with those. These findings have led to new recommendations about how patients should be screened before treatment begins.
Rheumatoid Arthritis Drugs: DMARDs.
Your physician may advise that you simply start treatment within a couple of months of identification with one of several types of DMARDs, should you’ve been identified as having rheumatoid arthritis. Among the most crucial drugs for treating rheumatoid arthritis, in the arsenal, DMARDs can often slow or stop the progression of RA by interrupting the immune process that encourages inflammation. Yet, they may take around half a year to be fully successful.
The quality of life has substantially enhanced for a lot of individuals with rheumatoid arthritis. These RA drugs are often used along with NSAIDs or glucocorticoids; however, with this kind of medicine, you may not need other anti-inflammatories or analgesics.
Because the immune system is targeted by DMARDs, they may also weaken the immune system’s ability to fight infections. This means you must be watchful for early signs of illness. Sometimes, you may even need regular blood tests to make sure the drug is just not hurting certain organs for example your liver, lungs, or kidneys or blood cells.
| Name | Brand Name(s) | Precautions | Potential Side Effects |
| auranofin (oral gold) |
Ridaura | Limit exposure to sun and tell your physician for those who have had:— Any adverse reactions to gold-including drugs — A history of blood cell issues — Inflammatory bowel, kidney, or bowel disorder |
— Low blood counts — Metallic flavor — Mouth ulcers — Skin rash or itching– Diarrhea |
|
azathiaprine |
Imuran |
Tell your doctor if: |
• Fever or chills Rare: Azathiaprine is associated with certain cancers, such as lymphoma. |
|
cyclosporine |
Sandimmune, Neoral |
Tell your doctor if you have: |
• Headache Increased risk of infection and certain cancers. |
| gold sodium thiomalate (injectable gold) |
Myochrysine |
Tell your doctor if you have: |
• Irritated, sore tongue Joint pain may occur for a few days after first few injections. |
| hydroxyChloroquine sulfate | Plaquenil | Tell your doctor if you have vision problems; vision may be damaged with high doses or long-term use. |
• Blurry vision or increased light sensitivity |
| leflunomide | Arava |
Tell your doctor if you have: Stop taking leflunomide before trying to conceive. |
• Dizziness |
| Methotrexate | Rheumatrex, Trexall | Tell your doctor if you have: • Abnormal blood counts • Liver or lung disease • Alcoholism • Active infection or hepatitis |
• Abdominal pain Rare, but serious: Dry cough, fever, or trouble breathing, which may result from a blood disease |
| tofacitinib | Xeljanz | • Xeljanz adds to risk of serious infections, cancers, lymphoma. • May increase cholesterol levels and liver enzymes. • May lower blood count. |
• Upper respiratory tract infection • Headache • Diarrhea • Inflammation of the nasal passage and the upper part of the throat |
Rheumatoid Arthritis Drugs: Biologic Response Modifiers.
Biologic response modifiers are a sort of DMARD. They target the part of the immune system response that leads to joint damage and inflammation. They help relieve symptoms and can boost your state as a result.
Rheumatoid arthritis can’t be cured by these RA medications. Symptoms may return if the drugs are stopped. But just as with other DMARDs, biologic response modifiers may slow the progression of the disease or help put it into remission. In case your physician prescribes one of these RA drugs, you’ll likely take it in combination with Methotrexate. Injection or by IV takes biologic response modifiers and so are pricey. Their long-term effects are not known.
NOTE: It is important to be tested for tuberculosis and hepatitis B and C. and to get proper vaccinations before taking biologics.
| Name | Brand Name | Precautions | Potential Side Effects |
| abatacept | Orencia | • Tell your doctor if you have a serious infection, such as pneumonia or COPD. • Do not take live vaccines. • Get tested for TB before starting treatment. |
• Cough • Dizziness • Headache • Serious infection • Infusion reaction • Serious infections, like TB, and infections from bacteria, viruses, or fungi |
| adalimumab | Humira |
• Tell your doctor if you have a serious infection, such as pneumonia. Get tested for TB before starting treatment. |
• Redness, pain, itching, or bruising at injection site • Upper respiratory infection • Serious infections, like TB, and infections from bacteria, viruses, or fungi |
| anakinra | Kineret | • Tell your doctor if you have a serious infection or a history of it. • Do not take live vaccines. |
• Redness, swelling, pain, or bruising at injection site • Serious infections, like TB, and infections from bacteria, viruses, or fungi |
| etanercept | Enbrel | Do not take if you have congestive heart failure, and tell your doctor if you have: • A serious infection • Been exposed to TB • A serious nervous system disorder • Do not take live vaccines. |
• Redness, pain, itching, swelling, or bruising at injection site Rare complications: • Serious infections, like TB, and infections from bacteria, viruses, or fungi |
| infliximab | Remicade | Tell your doctor if you have: • A serious infection, especially hepatitis B • Been exposed to TB • A serious nervous system disorder • Do not take live vaccines. |
• Chest pain Rare complications: • Serious infections, like TB, and infections from bacteria, viruses, or fungi |
| rituximab | Rituxan | • Tell your doctor if you have a serious infection, or heart or lung disease. • Do not take live vaccines. |
• Abdominal pain Serious side effects: • Serious infections, like TB, and infections from bacteria, viruses, or fungi |
| golimumab |
Simponi Simponi Aria |
• Tell your doctor if you have any infections or health conditions, like heart disease, MS, or diabetes• Get tested for TB before starting treatment. • Do not take live vaccines. • See your doctor right away if you develop signs of infection while taking this drug. |
• Redness at the injection site Rare complications: • Serious infections, like TB, and infections from bacteria, viruses, or fungi |
| certolizumab pegol | Cimzia | • Tell your doctor if you have an infection or are being treated for an infection, or if you have diabetes, HIV, hepatitis B, cancer, or TB. | • Heart failure • Nerve problems such as MS • Allergic reactions • Autoimmune problems like lupus • Reactivation of hepatitis B • Serious infections, like TB, and infections from bacteria, viruses, or fungi |
| tocilizumab | Actemra | • Tell your doctor if you have a serious infection, history of gastrointestinal perforation, or if you are pregnant or plan on becoming pregnant. • Do not take live vaccines. |
• Upper respiratory tract infection • Inflammation of the nose or throat • High blood pressure • Headache • Abnormal liver enzyme level • Serious infections, like TB, and infections from bacteria, viruses, or fungi |
Rheumatoid Arthritis Drugs: Glucocorticoids.
Glucocorticoids are steroids. They’re powerful anti-inflammatory drugs that may also block other immune responses. These rheumatoid arthritis medications help alleviate symptoms and may prevent or slow joint damage. These RA drugs are received by you by injection, or by pill.
Due to the chance of negative effects, you must only use these RA drugs for example, for brief periods, until DMARDs reach their full effectiveness or when disease flares up. If your side effects are serious, do not cease taking the drug suddenly. Speak about what to do first with your doctor.
| Name | Brand Name(s) | Precautions | Potential Side Effects |
|
Betamethasone injectable |
Celestone | Tell your doctor if you have: • Fungal infection • History of TB • Underactive thyroid • Diabetes • Stomach ulcer • High blood pressure • Osteoporosis |
• Bruising • Cataracts • Increased cholesterol •Atherosclerosis • High blood pressure • Increased appetite or indigestion • Mood swings or nervousness • Muscle weakness • Osteoporosis • Infections |
|
Prednisone |
Ravos | Tell your doctor if you have: • Fungal infection • History of TB • Underactive thyroid • Diabetes • Stomach ulcer • High blood pressure • Osteoporosis |
• Bruising • Cataracts • Increased cholesterol •Atherosclerosis • High blood pressure • Increased appetite or indigestion • Mood swings or nervousness • Muscle weakness • Osteoporosis • Infections |
Rheumatoid Arthritis Drugs: NSAIDs.
NSAIDs work by blocking. By reducing inflammation, NSAIDS help reduce swelling and pain. But they are ineffective in reducing joint damage. These drugs are ineffective in treating the disease. They ought to be taken together with other rheumatoid arthritis medications.
As with glucocorticoids, you need to use them for brief periods — they may cause severe digestive tract issues. Which sort, if any, your physician prescribes may depend upon your medical history. It’s best not to take these drugs, when you have a history of stomach ulcers or liver, kidney, heart problems. Ask your doctor whether any new NSAIDS creating fewer side effects can be found.
| Name | Brand Name(s) | Precautions | Potential Side Effects |
| celecoxib | Celebrex | • Tell your doctor if you have had a heart attack, stroke, angina, blood clot, or high blood pressure or if you have sensitivity to NSAIDS or sulfa drugs. • Do not take with other NSAIDS. • Do not take late in pregnancy. |
• Increased risk of heart attack and stroke Indigestion, diarrhea, and stomach pain |
|
Diclofenac sodium |
Voltaren |
Tell your doctor if you: |
• Abdominal cramps, diarrhea Greater risk of complications for people with cardiovascular disease |
| Ibuprofen | Motrin, Advil |
Tell your doctor if you: |
• increased risk of heart attack and stroke Abdominal cramps, diarrhea Greater risk of complications for people with cardiovascular disease |
Rheumatoid Arthritis Drugs: Analgesics.
Pain is reduced by analgesics but they cannot reduce joint damage or swelling.
There really are a variety of over-the-counter and prescription analgesics. Narcotics would be the strongest kind of analgesic. Use these carefully and make sure you let your doctor know when you have any history of alcoholism or drug abuse.
| Name | Brand Name(s) | Precautions | Potential Side Effects |
| acetaminophen | Tylenol, Faverall | • Tell your doctor if you have 3 or more drinks of alcohol daily. • Avoid taking more than one product with acetaminophen. |
Side effects uncommon if taken as directed. |
|
tramadol |
Ultram |
• Tell your doctor if you use central nervous system depressants, tranquilizers, sleeping medications, muscle relaxants, or narcotic pain medications or if you have a history of drug or alcohol abuse. • Do not drive or use heavy machinery until you know how your body reacts to the drug. |
• Constipation • Diarrhea • Drowsiness • Increased sweating • Loss of appetite • Nausea |
| oxycodone | OxyContin, Roxicodone |
Tell your doctor if you use central nervous system depressants, tranquilizers, sleeping medications, muscle relaxants or narcotic pain medications or if you have a history of drug or alcohol abuse. |
• Constipation • Dizziness • Drowsiness • Dry mouth • Headache • Increased sweating • Itchy skin • Nausea or vomiting • Shortness of breath |
Diet, Exercise and Rehabilitation Services
Locating a balance between rest and exercise is essential to managing rheumatoid arthritis. Rest and take it easy — when your joints are sore, warm and bloated — when your symptoms flare up. You can continue to do range-of-motion exercises to maintain your joints mobile, but be careful to not tire yourself or aggravate your joints. Avoid walking, housework or other activities that are unneeded. When other symptoms, including fatigue and morning stiffness, are much less noticeable and when your joints feel better, raise your activity. Weight-bearing exercises like walking and lifting weights can fortify weakened muscles without risking additional joint damage. Cut back a little if exercise produces more pain or joint swelling.
Despite many claims, there are no dietary changes, supplements, herbs or other alternative therapies known to improve the symptoms of rheumatoid arthritis over a long amount of time. Nevertheless, a diet that assists you to lose excess weight may be beneficial for weight bearing joints affected by rheumatoid arthritis.
Having rheumatoid arthritis often implies that you must pay particular focus on the way you move. An occupational therapist or physical therapist will offer guidance and suggestions as you handle ordinary tasks around your home and work. Additionally, unique apparatus that will help you conserve energy and protect your joints throughout your daily activities can be provided by a therapist. A sling, brace, splint or Ace bandage when your joints are specifically vulnerable, worn can take the pressure and shield them from injury. A podiatrist may supply shoe inserts (orthotics) or even suggest operation to enhance pain and function in arthritic feet.
Surgery
In some cases, surgery is necessary to get rid of inflamed tissue, or to reconstruct or replace the affected joint. Arthroplasty, a surgical procedure to replace the joint, may be a highly effective choice when rheumatoid arthritis causes major destruction and pain in the hip or knee. Especially surgical tendon repair might be recommended, because rheumatoid arthritis can cause tendon damage.
When To Call A Professional
Tell your doctor in case you experience any of the following:
- Occasional fever
- Pain or stiffness in the morning (lasting more than 30 minutes)
- Issues in symmetrical joints (both knees, as an example)
- Exhaustion
Prognosis
Effective treatment can assist you to live well with rheumatoid arthritis, even though the intensity of its own response to therapy and the disease are highly changeable.