Last Updated on April 28, 2023
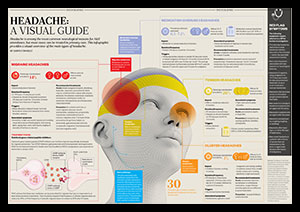
Gloria Pope, director of advocacy and public policy for the Depression and Bipolar Support Alliance, says she can feel her depression being fueled by them and suffers excruciating migraine headaches.
“I go all week under stress, and when it’s the weekend, the headaches smack me,” says Pope. She says she loses the equivalence of two because she’s afraid she’ll be hit with a huge head ache, she does not make strategies. As summer and pleasant weather tactic, she’s says it brings her down to be stuck inside, “sick as a dog.”
Persistent pain as well as depression are closely associated — so much so that physicians often aren’t quite sure which condition causes the other. Depression happens at least three times more often in those who deal with chronic pain than in individuals who actually don’t. Research indicates that if all patients with persistent pain were screened for depression, many instances of undiagnosed depression would be found.
The Depressing Side of Pain
According to researchers, there are a number of reasons why long-term pain and depression are so closely linked:
- Chronic pain takes an emotional cost. When you’re in pain all of the time, you’re not able to take care of your day-to-day responsibilities as readily as well as your relationships with family and friends may become strained. Not surprisingly, studies have discovered that the level of pain a person experiences directly influences symptoms of depression — more physical pain only takes a larger price on your own mood.
- Exactly the same regions of the brain regulate pain as well as melancholy. Researchers have discovered that the same regions of the brain are accountable for processing both pain and feelings of depression. Another study revealed the part of the mind that works to reduce pain was sluggish in the blue subjects. The brain uses many of the same substances responsible for regulating disposition, including norepinephrine and serotonin, to transmit pain signals. Chronic pain and melancholy that is chronic both have similar influences on the nervous system as well, often intensifying perceptions of pain. It is no coincidence that many drugs prescribed as antidepressants are effective in treating pain, also.
Treating Pain and Depression Together
A mixture of therapies is normally necessary to treat persistent pain occurring in association with melancholy. The physical source of your pain must be medicated along with your feelings of depression.
Treatments your doctor might recommend to help you cope with pain and melancholy include:
- Pain medication
- Antidepressants
- Massage
- Meditation
- Biofeedback
- Hypnosis
- Cognitive-behavioral therapy
- Psychotherapy
An individual experiencing depression and chronic pain might additionally benefit from treatment in a pain management facility. Specialists at these centres are skilled at combining the therapies listed above to help break the cycle by which symptoms of pain and melancholy feed off each other.
Successful treatment of chronic pain and depression can be quite a drawn-out process. You may need to try many different therapies before finding one that copes with your depression and helps relieve your pain. Be patient and remember that both states could be handled effectively.